Introduction
Votre bébé est hospitalisé dans notre service et vous désirez l’allaiter. Ce guide vous aidera tout au long de votre séjour en néonatologie et lors de votre retour à domicile.
Nous serons là pour vous accompagner et vous soutenir dans votre choix.
Les avantages de l'allaitement chez l'enfant prématuré
- Le lait maternel facilite la mise en route du transit intestinal. Les composants du lait maternel sont parfaitement adaptés à la digestion et à la croissance de votre bébé.
- Le lait maternel contient de très nombreux facteurs de défense. Ces facteurs ont une action locale au niveau du tube digestif, ils ont également un effet dans tout le corps renforcé par la pratique du kangourou. Votre lait protège votre enfant du risque d’infection et du risque d’allergie.
- Le lait maternel aide au bon développement des fonctions neurologiques, visuelles et psychomotrices.
- Il est démontré que la maîtrise de la succion-déglutition-respiration est meilleure au sein qu’au biberon. Les bébés sont plus stables, ils font beaucoup moins d’apnées et de bradycardies.
- Le fait de donner son lait à son bébé est pour la mère une opportunité de partage avec son bébé.
Les avantages écrits ci-dessus font que les bébés nourris au lait maternel se développent bien, sans excès de poids et sont moins souvent malades que les bébés nourris au lait artificiel.
Allaiter est non seulement idéal au niveau nutritionnel mais également au niveau du développement affectif du bébé.
Les différentes étapes
Observez bien le comportement de votre bébé. En fonction de son âge et de son état d’éveil ses compétences seront différentes. Au début de l’apprentissage, nous serons strictes sur la fréquence et la quantité des repas. Doucement nous nous adapterons aux rythmes de votre bébé pour arriver à un allaitement à la demande. Nous profiterons du moment
de la tétée pour compléter votre bébé.
Le sein de contact
Premier contact avec sa maman, se voir, se parler, se toucher, se sentir, le peau à peau (méthode kangourou) pour créer le contexte de la mise au sein. Il est préférable de tirer votre lait avant le kangourou ou les tétées de contact pour profiter pleinement de ce moment, sans interruption.
La tétée d’apprivoisement
Pour «apprendre» le sein : être contre le sein et le mamelon de sa maman même sans rien téter (ou s’endormir) pour la chaleur, l’odeur, la vue, le goût du sein, du lait.
La tétée d’apprentissage
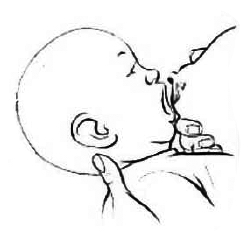
Pour apprendre à téter : le bébé ouvre la bouche, attrape le sein mais a du mal à le garder en bouche ou il tète 2-3 fois puis s’endort. Il peut déclencher les flux («le lait vient») mais il a du mal à entretenir les flux. Soutenez votre sein pour qu’il puisse le garder en bouche. Afin de ne pas trop fatiguer votre bébé, limitez la tétée à 30 minutes. Après la tétée, n’oubliez pas de recueillir votre lait.
La tétée nutritionnelle
Le bébé prend bien le sein en bouche et arrive à le garder avec un minimum d’aide, la langue est sortie autour du mamelon. On voit le bébé téter longuement et on l’entend déglutir. Au début, nous pèserons avant et après la mise aux seins pour voir combien votre bébé a mangé. Petit à petit, votre bébé va arriver en allaitement à la demande, c’est-à-dire qu’il peut boire ce qu’il veut aussi souvent qu’il veut, il n’a plus d’heure imposée.
Nous vous proposons «une fleur de lait» qui consiste à suivre l’évolution, les progrès de votre bébé. Chaque semaine, vous pouvez colorier les pétales de la fleur correspondant au comportement de votre enfant.
Dès que l’état de santé de votre bébé le permet, vous pouvez le mettre au sein.
La mise aux seins
La position pour bien allaiter est très importante pour prévenir les crevasses et le bon déroulement du repas. Laissez-vous le temps, laissez-lui le temps d’apprendre, de découvrir, de chercher le sein.
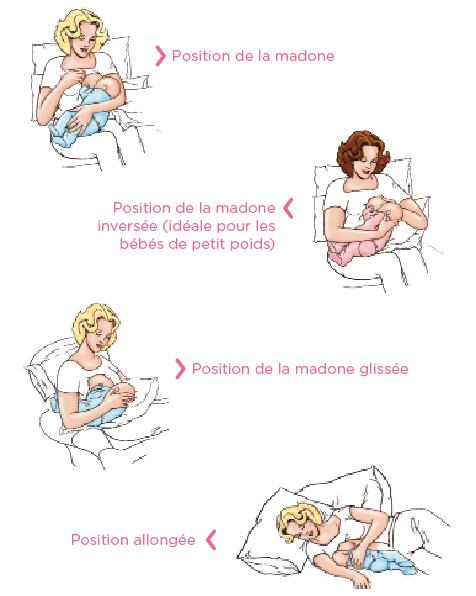
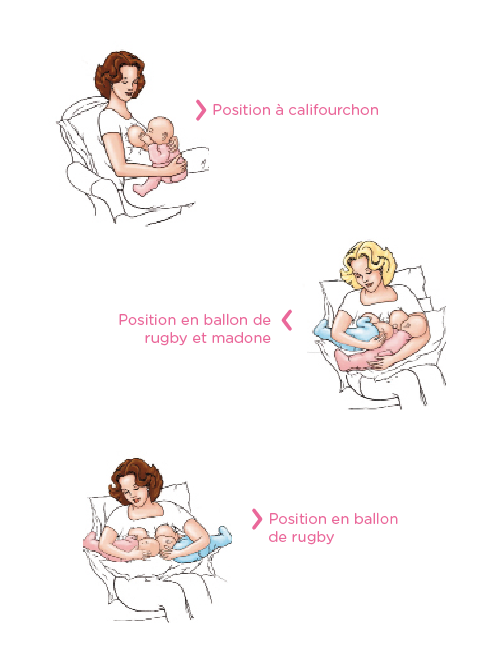
Au fur et à mesure de l’apprentissage, nous vous montrerons les différentes positions et vous pourrez choisir celle qui vous convient le mieux.
Il est important d’alterner les côtés à chaque tétée. Présentez le sein aussi longtemps qu’il veut et proposez le deuxième sein. Si vous donnez les 2 seins commencez par le dernier présenté lors de la dernière tétée.
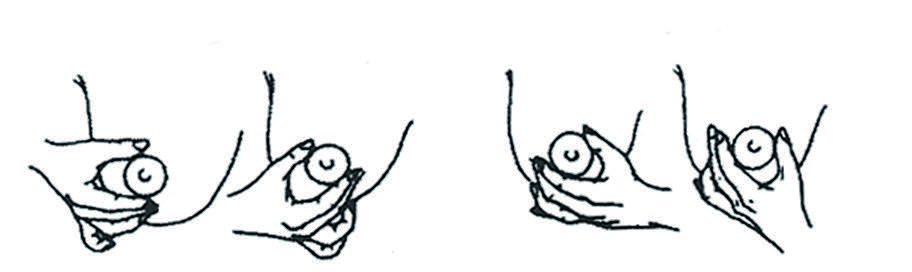
1. Installez-vous confortablement, assise, bien calée avec des coussins. Le corps du bébé doit être très proche du vôtre (ventre contre vous).

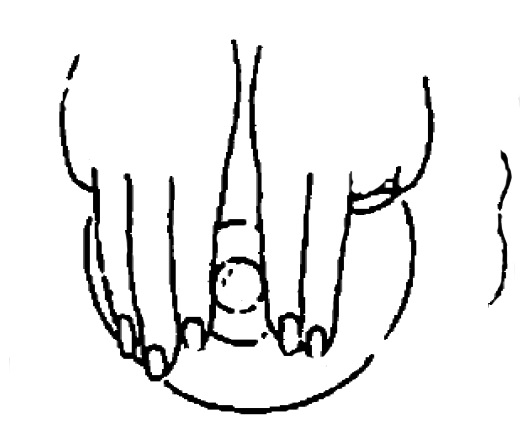
2. Touchez la lèvre supérieure du bébé avec le mamelon. Dès qu’il ouvre la bouche bien grande, amenez votre bébé au sein et placez lui l’aréole bien en bouche afin qu’il puisse l’attraper et la garder.
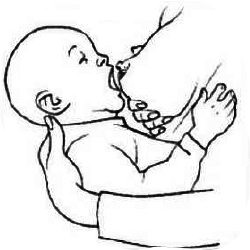
3.Soutenez votre sein avec la main (ne le lâchez pas trop vite pour que le bébé puisse bien l’attraper et ne le perde pas).
4. La bouche grande ouverte, votre bébé doit prendre le mamelon mais aussi une grande partie de l’aréole, la lèvre inférieure étant bien recourbée vers l’extérieur, la langue est sortie et masse l’aréole (ceci est très important pour la stimulation).
5. Attirez bien ses fesses vers vous, ainsi le nez reste dégagé.
Positions pour l'allaitement
Assouplissement auréolaire
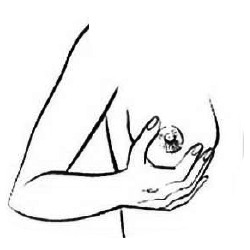
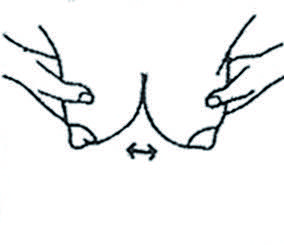
Si votre sein est trop tendu, vous pouvez effectuer un massage aréolaire avant de mettre votre bébé au sein.
L’oedème du mamelon apparaît en général entre 2 à 3 jours après l’accouchement. Il est encore plus important lors de la «montée de lait».
Le but du massage aréolaire est d’assouplir votre mamelon pour faciliter la prise du sein pour le bébé. Plus l’aréole est ferme ou enflée, plus il faudra du temps pour l’assouplir.
Le massage aréolaire est nécessaire lorsque le mamelon et l’aréole sont enflés et durs afin de faciliter la prise du sein par le bébé.
Il existe 3 techniques différentes. Vous utilisez celle qui vous convient le mieux et avec laquelle vous êtes le plus à l’aise :
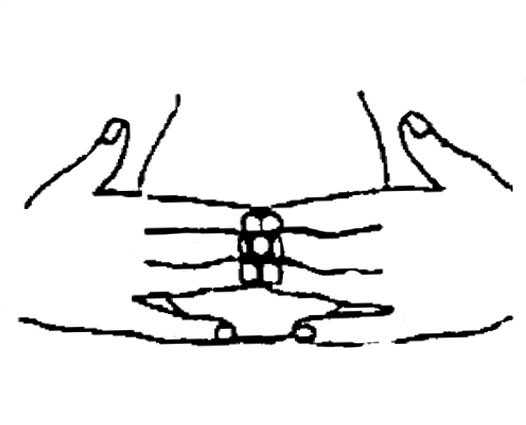
1. En 2 étapes, appuyer à la base du mamelon et pivoter d’un quart de tour.
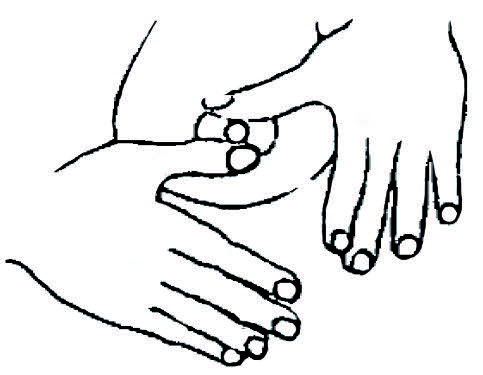
Puis changer la position des mains.
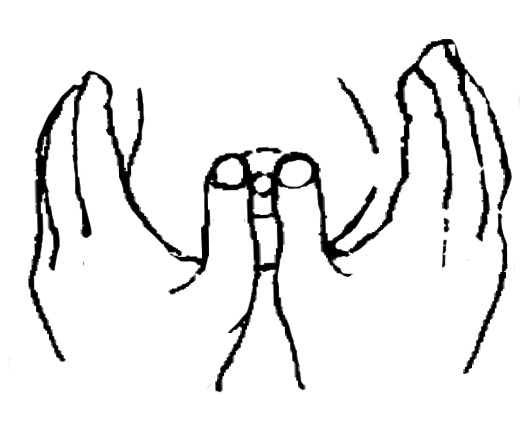
2. En 1 étape, appuyer à la base du mamelon avec 3 doigts de chaque main.
3. En 2 étapes, pivoter d’un quart de tour 2 ou 3 doigts de chaque côté. Répéter avec les doigts au-dessus et en-dessous du mamelon.
Pourquoi pomper le lait maternel?
Malheureusement, pour diverses raisons, votre bébé est dans l’incapacité de prendre le sein ou ne le stimule pas assez. Il est dès lors nécessaire de passer par l’étape du tire-lait. Ce passage obligé va permettre à votre corps d’établir le début de la production de lait.
Votre lactation est établie mais votre enfant ne sait pas aller au sein. Il vous faut tirer le lait pour maintenir une bonne production de lait maternel. Dans ce cas, le but est de produire suffisamment de lait maternel pour subvenir aux besoins de votre bébé. A titre informatif, 500 ml de lait maternel par jour à la troisième semaine est une bonne moyenne.
Vous désirez pouvoir vous absenter et offrir à votre enfant le bénéfice du lait maternel. Nous parlons alors de l’établissement d’une réserve de lait maternel.
Vous prenez des médicaments qui ne vous permettent pas d’allaiter. Dans ce cas, vous tirez votre lait pour maintenir la production de lait le temps de votre traitement. Malheureusement vous devez alors le jeter.
De quel matériel ai-je besoin?
Le matériel que vous utilisez doit être confortable et efficace. Il doit également être facile à monter, nettoyer et utiliser.
Le tire-lait manuel
Il s’utilise facilement sans contrainte de source d’électricité. Facilement transportable de par sa taille, il vous accompagne dans vos déplacements. Les cycles d’expression se font en fonction de votre rythme. La pression d’expression du lait se régule par la force que vous utilisez pour actionner la poignée. Il est à conseiller lorsque la lactation est établie ainsi que pour des périodes courtes et/ou épisodiques.
Le tire-lait électrique
Il s’utilise dès les premières heures suivant l’accouchement et durant toute la période nécessaire. Pratique, la pression d’expression se règle de façon automatique à l’aide d’un bouton. Il n’y a donc pas de variation de pression durant tout le cycle si vous ne le désirez pas. Les cycles sont réguliers en nombre et en durée.
Leur coût à l’achat est élevé. Vous pouvez en louer dans les pharmacies et les points de prêt de matériel médical (ex.: Hospilux). Le tire-lait électrique est l’idéal pour l’établissement de la lactation ainsi que pour le long terme. Il existe des doubles tire-lait (possibilité de pomper les deux seins en même temps). Nous les conseillons car il diminue le temps d’expression par deux et la stimulation est double et simultanée, il augmente la quantité de lait produite. Si vous vous procurez un simple tire-lait électrique c’est très bien aussi. La seule fonction de l’appareil qui soit indispensable est la force de pression ajustable. Achetez celui qui vous convient le mieux.
L’embout
Il doit être CONFORTABLE pour empêcher les lésions et suffisamment adapté pour assurer l’étanchéité. Il doit être nettoyable et stérilisable. De nombreux modèles sont disponibles sur le marché. Achetez celui qui vous convient le mieux en vous assurant qu’il soit compatible avec votre tire-lait. Il est nécessaire d’en acheter minimum 2 (Ce matériel ne se loue pas).
La bouteille
Elle doit être compatible avec votre matériel. De préférence en plastique (le verre casse!) et graduée, elle vous permettra d’évaluer la quantité que vous produisez. Elle n’est pas à usage unique mais est nettoyable et stérilisable.
Avec un couvercle à visser, elle doit être étanche. L’idéal est de pouvoir y adapter une tétine afin d’éviter de manipuler votre lait lorsque vous voulez le donner à votre bébé. La bouteille sera étiquetée avec la date et l’heure de l’expression du lait. Ne remplir les bouteilles que jusqu’à la dernière graduation.
Quand tirer le lait, à quelle fréquence et pendant combien de temps?
Il faut tirer le lait maternel de préférence juste après une tétée et à intervalles réguliers. Si votre bébé a un rythme d’alimentation fixe (ex: lors d’une hospitalisation), le mieux est de tirer votre lait au même rythme.
La fréquence minimale est de 8 fois par jour et ce MêME LA NUIT. En effet, la nuit les taux hormonaux sont plus élevés et stimulent mieux la production de lait maternel. Plus les quantités de lait que vous pompez sont petites, plus souvent il vous faudra tirer. Sachez que la fréquence influence le volume de lait.
Durant les premiers jours et ce jusqu’à la production de lait proprement dite (environ 1 semaine), il est conseillé de pomper au minimum 15 minutes chaque sein toutes les 3-4 heures. Par la suite, il vous faudra pomper jusqu’à 2 minutes après le flux de lait.
Comment entretenir mon matériel?
Se laver les mains avant chaque manipulation.
La pompe doit être entièrement démontée et nettoyée à l’aide d’un chiffon et d’eau savonneuse 1x/semaine. Les parties stérilisables doivent aussi l’être 1x/semaine. Vous le ferez plus souvent si cela s’avère nécessaire.
L’embout et ses composants doivent être démontés après chaque usage. Ils sont alors nettoyés à l’eau savonneuse (aucune trace de lait ne doit persister), soigneusement rincés à l’eau claire et laissés sécher à l’air libre sur un linge propre et sec et à l’abri de la poussière. A domicile, l’embout est stérilisé 1x/jour.
Les bouteilles sont soigneusement nettoyées et stérilisées après chaque usage. Les sachets collecteurs sont à usage unique. Les tétines, bagues et capuchons sont soigneusement nettoyés et stérilisés après chaque usage.
Comment donner mon lait à mon enfant?
Le lait qui vient d’être pompé ne doit pas être réchauffé et peut être donné directement à votre bébé.
Les techniques pour alimenter votre bébé sont diverses. Si votre enfant n’a pas encore de succion efficace au sein, il est déconseillé de donner le biberon. Il vous reste l’alternative de l’alimentation à la tasse et à la seringue.
Ces techniques restent cependant difficiles à appliquer. Elles doivent vous être enseignées par une personne qualifiée. Lorsque votre bébé prend le sein de manière efficace, vous pouvez donner le biberon.
Le lait maternel qui est réfrigéré, doit être réchauffé. Vous le faites dans un chauffe-biberon ou au bain-marie. Evitez le plus possible le micro-onde car il altère les qualités nutritionnelles de votre lait.
Après avoir réchauffé votre lait, n’oubliez jamais de vérifier sa température avant de le donner à votre enfant.
Comment conserver mon lait maternel et combien de temps?
Pour une bonne conservation du lait maternel, la première règle est l’hygiène.
N’oubliez pas d’inscrire, sur les récipients et de manière ineffaçable, la date et l’heure d’extraction de votre lait maternel.
Pour transporter du lait maternel, il faut le mettre dans un sac isotherme ou une glacière. Dès que possible, remettez-le au réfrigérateur.
Le lait maternel réchauffé doit être donné dans l’heure qui suit son réchauffement ensuite il sera jeté. Le lait réchauffé une fois et refroidi DOIT être jeté.
Le lait maternel fraîchement pompé peut être conservé à température ambiante maximum 4 heures et maximum 1 heure dans une pièce dont la température est supérieure à 22°. Si vous ne donnez pas votre lait tout de suite après l’avoir tiré, il faut le mettre au réfrigérateur.
Dans une glacière réfrigérée, le lait maternel frais peut être conservé maximum 24 heures. Au réfrigérateur, le lait maternel frais se conserve au maximum 72 heures (=3 jours). Le lait maternel décongelé, même conservé au réfrigérateur, sera éliminé après 24 heures.
Pour conserver du lait maternel plus longtemps, il faut nécessairement le congeler. Dans le compartiment congélation (freezer, bac à glaçon) de votre réfrigérateur, le lait maternel se conserve au maximum 2 semaines. Dans un congélateur «grand format» ou dit «séparé» à une température de minimum -20°, votre lait peut se conserver maximum 12 mois. Si votre congélateur ne refroidit pas à -20°, le lait maternel se conserve maximum 6 mois.

Expression manuelle du lait
Pourquoi exprimer manuellement son lait?
- Le tire-lait mécanique est inefficace et/ou inconfortable.
- La maman préfère cette méthode plus naturelle.
- La méthode est pratique, gratuite et écologique.
- Pour donner son colostrum lorsqu’on est séparé de son bébé.
- Pour soulager une tension mammaire.
- Pour aider son bébé en induisant l’écoulement du lait.
- Pour éviter un engorgement des seins.
- Pour stimuler, augmenter ou maintenir la production de lait.
La technique
La technique dite Marmet a été mise au point par une mère qui a du exprimer son lait pendant une longue période.
C’est une méthode qui allie massage et stimulation afin de favoriser la production et le réflexe d’éjection du lait. Cette technique est efficace et ne provoque aucun problème. Comme toute technique, elle demande un peu d’expérience et d’application pour montrer toute son efficacité. Elle est cependant très facile à apprendre.
La durée
Toute l’opération devrait prendre 20 à 30 minutes lorsque l’expression manuelle remplace une tétée.
- Exprimer du lait de chaque sein pendant 5 minutes.
- Masser, caresser, secouer pendant 1 minute.
- Exprimer du lait de chaque sein pendant 5 minutes.
- Masser, caresser, secouer pendant 1 minute.
- Exprimer du lait pendant 3 minutes.
Ces durées sont à titre indicatif. Elles doivent être suivies si il n’y a pas encore ou peu de lait. Si la production de lait est bien établie, observer le débit d’écoulement et changer de sein dès que celui-ci diminue. Chaque partie de la technique peut-être répétée seule et au besoin.
Les soignants vous guideront et conseilleront tout au long de votre apprentissage. Nous restons à votre disposition pour toute question complémentaire.
Techniques :
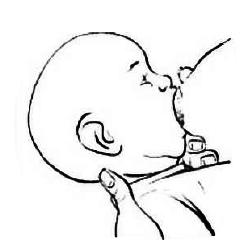
1. Placer le pouce, l’index et la majeur sur le sein, à environ 3 cm de la base du mamelon. Le pouce sur le dessus du mamelon et les 2 autres doigts sur le dessous tel qu’illustré. Eviter d’entourer le sein.
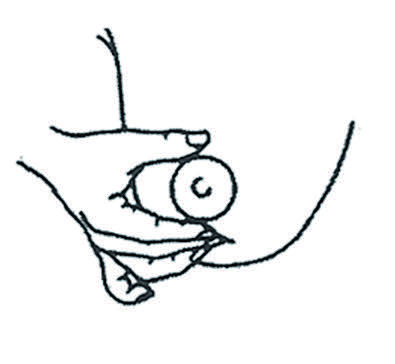

Adopter une position en C, ne pas entourer le sein.
2. Appuyer fermement les doigts contre la cage thoracique. Eviter d’écarter les doigts. Si les seins sont volumineux, soulever-les avant d’appuyer contre le thorax.

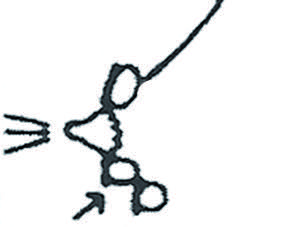
Pousser contre la cage thoracique, rouler puis finir le mouevment de roulement.
3. Rouler le pouce vers l’avant comme la prise d’empreinte digitale. Pendant ce temps transférer la pression du majeur à l’index. Répéter la séquence en cadence. Déplacer le pouce et les doigts afin de drainer d’autres parties du sein en observant la position des doigts.
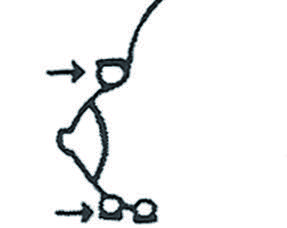
4. Éviter de comprimer, tirer ou glisser sur le sein car cela peut entraîner des lésions.

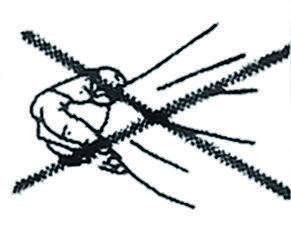

Ne pas comprimer, tirer ou glisser.
5. Pour faciliter l’écoulement du lait, masser les glandes et les canaux qui sécrètent le lait. Caresser doucement la surface du sein de haut en bas. Secouer doucement le sein, penchée vers l’avant.


Masser, caresser et secouer.
Est-ce que mon lait est bon pour mon bébé?
Lorsque l’enfant naît prématurément les qualités du lait maternel conviennent parfaitement pour son développement et pour sa protection face aux infections.
Cependant, ses besoins sont tels qu’il faut légèrement supplémenter le lait en protéines pour favoriser sa croissance. La composition du lait s’adapte à l’âge de l’enfant et varie en cours de tétée. Ces modifications sont à l’origine des variations de l’aspect du lait. Le lait maternel n’a pas toujours la même saveur. Il est d’abord désaltérant en début de tétée puis plus riche, il a le goût de ce que vous mangez. Votre lait évolue en même temps que votre bébé, il est toujours adapté à son âge et à ses besoins.
Votre lait changera d’aspect et de couleur, il deviendra bleuté, c’est normal. Vos seins deviendront souples mais ils produiront toujours autant de lait. C’est ainsi qu’évoluent normalement les seins de toute femme allaitante.
Comment me nourrir?
Vous pouvez manger de tout en quantité raisonnable, comme pendant la grossesse, la variation du goût de votre lait enchantera aussi votre bébé.
N’oubliez pas qu’il a apprécié le goût déjà pendant la grossesse. Aucun aliment ne doit être écarté d’office si vous vous nourrissez de manière variée et équilibrée, par exemple des légumes frais, des produits laitiers, du poisson, des viandes maigres, du pain complet. Buvez pour étancher votre soif. Évitez l’alcool, le tabac et les excitants.
Ai-je assez de lait?
Sachez que les trois premiers jours vous n’avez pas de lait mais du colostrum en petite quantité qui correspond à la capacité de l’estomac du bébé. Le colostrum est très important, il contient beaucoup d’anticorps et est très nourrissant.
Au-delà de 3 jours, l’allaitement se met en route (voir 7 jours en cas de césarienne).
Jusqu’à trois semaines c’est du lait de transition, après trois semaines c’est un lait dit mature. Les baisses réelles de productions ne sont pas fréquentes. La demande règle l’offre, téter ou tirer son lait stimule la sécrétion lactée.
C’est la fréquence des tétées (ou du tire-lait) plus que la durée qui augmente la production de lait. En cas de baisse de production il faut donc tirer son lait plus souvent, si possible près du bébé ou avec une photo de lui près de soi en cas de séparation.
Il est tout à fait normal qu’un enfant réclame plus souvent pendant les périodes de croissance. Celles-ci se situent entre 7 et 10 jours de vie, entre 6 et 8 semaines et vers 3 mois. Pendant ces périodes, l’enfant a beaucoup plus faim, allaitez le plus fréquemment, la production de lait va s’adapter aux besoins supplémentaires.
Est-ce que mon lait est bon pour mon bébé?
L’engorgement des premiers jours est normal, c’est la montée laiteuse. Elle peut être diminuée par une mise au sein précoce et des tétées fréquentes ou par l’utilisation du tire-lait plus fréquente.
Pour vous soulager en cas de douleur, commencez par proposer le sein ou par utiliser le tire-lait. Vous pouvez en plus prendre une douche ou appliquer des compresses chaudes ou froides et masser l’aréole.
Dans la plupart des cas cela fera couler le lait qu’il vous sera possible de recueillir dans un biberon. Par la suite les seins peuvent encore être engorgés lorsque vous avez mal vidé vos seins.
Comment éviter et soulager les mamelons douloureux?
Vérifier la bonne position de votre bébé. Évitez tout ce qui pourrait dessécher et altérer l’odeur du mamelon (savon, alcool, désinfectant,…). Après la tétée, étendez sur le mamelon et l’aréole une goutte de lait maternel, cicatrisant et protecteur et laissez le sécher à l’air.
Lors des premières tétées, il se peut que vous ressentiez des sensations désagréables : tiraillements ou pincements au niveau des mamelons. C’est tout à fait normal et cela ne devrait pas durer. Si les douleurs persistent pendant la tetée, n’hésitez pas à nous contacter.
Comment savoir s’il a assez bu?
L’enfant peut être pesé si l’on a besoin de savoir exactement combien il a bu. Ses couches doivent être bien mouillées (car plus il boit, plus il fait pipi), il doit uriner 4 à 5 fois par jour, et faire des selles 1x par jour.

Qu’est-ce que la préférence sein-tétine?
Le bébé ne boit pas au sein comme au biberon, les techniques sont différentes. Au sein, il doit sortir la langue et masser l’aréole pour avoir du lait, au biberon, la langue peut rester dans la bouche, il recevra son lait.
Pour limiter cette confusion, la tasse, la petite cuillère et le dispositif d’aide à l’allaitement doivent être préférées au biberon.
Pour réussir un allaitement et limiter la confusion votre présence est très importante, l’idéal est que vous soyez là le plus souvent possible pour les tétées. Si le bébé apprend à boire au biberon avant le sein, il tétera avec la langue rentrée et ne massera pas l’aréole, il risque de ne pas déclencher les flux quand il sera au sein. Il est donc préférable qu’il apprenne d’abord à boire au sein puis au biberon.
Est-ce que mon enfant a la diarrhée?
Les enfants nourris aux seins souffrent rarement de diarrhées. Les selles sont de consistances onctueuses ou liquides et peuvent contenir des grumeaux. Elles sont d’un jaune ocre et la couleur peut varier selon l’alimentation de la maman. La quantité et la fréquence de selles peut varier au cours de l’allaitement ; il peut avoir des selles à chaque change ou qu’1 fois par jour.
Pourquoi mon bébé pleure?
Le bébé a différentes raisons de pleurer : faim, coliques, besoins de câlins, trop chaud, trop froid… C’est son seul moyen de s’exprimer.
Il est important de répondre à ses pleurs, surtout n’hésitez pas à le prendre dans vos bras, lui faire un câlin et lui parler. Vous pouvez aussi le porter en écharpe, il ne sera pas gâté pour autant, vous répondrez seulement à ses besoins.
J’ai l’impression que mon bébé tête moins bien
Il est possible que les progrès de votre bébé ne soient pas constant. Il est petit et immature et a beaucoup d’acquisitions à faire. Vous risquez de vous décourager face à son apprentissage qui parfois peut vous paraître lent mais chaque bébé a son rythme. S’il s’endort au sein, tête moins bien, c’est une phase de son apprentissage, continuez à l’encourager et ne perdez pas le moral.
À titre informatif : à la troisième semaine, 500 ml de lait maternel par jour est une bonne moyenne. Tenir un journal de votre quantité de lait recueilli sur 24h nous permet de voir une éventuelle diminution et agir en conséquence.
Toute l’équipe de soins du service de Néonatalogie reste à votre disposition en cas de doute ou de questions supplémentaires. N’hésitez pas à nous contacter au 4411 3157 si nécessaire.
